Case 5 Index
Introduction
ED Bounceback
Outcome
Nurse Depositions
Nurse Expert Witnesses
Physician Depositions
Physician Expert Witnesses
Legal Outcome
Documentation Review
Medical Review
For this case we will review the documentation of the second doctor to see the patient. In particular, we will review the note that was written after he fell and returned to the ED.
As usual, the Documentation Rubric will be used to grade the note. The Rubric is a tool to be used in hindsight; the Documentation Template exists to help guide physician in real-time, while working during a shift. It will help improve your notes and make a positive outcome more likely.
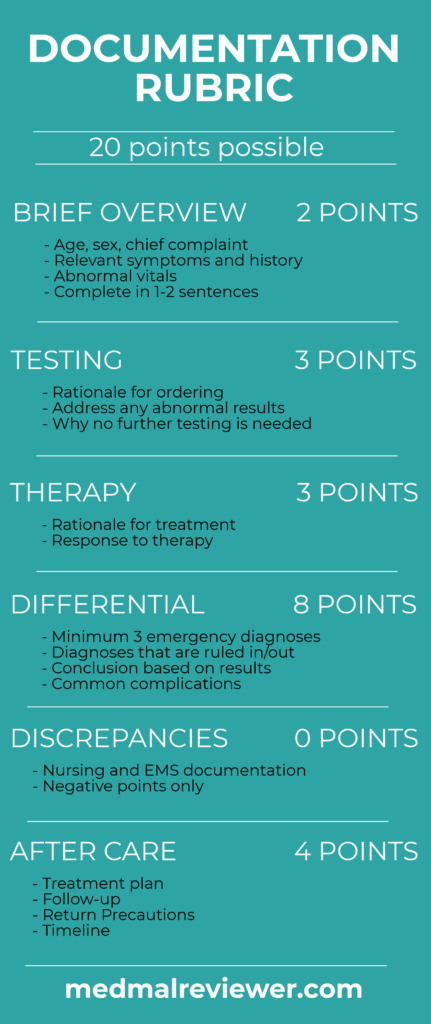
This case received a final score of 11.5/20.
The structure of this note is slightly atypical compared to most ED notes, which is influenced by the software used to write the note. It is built in a SOAP (subjective, objective, assessment, plan) format.
Brief Overview: 1/2
All of the necessary details are included in the history and physical exam, but there is no brief overview. The brief overview should be a 1-2 sentence description of the relevant facts, listed at the beginning of the MDM. While not absolutely necessary, it helps the physician synthesize the relevant facts, and helps anyone reviewing the chart later understand the most important information that was used to make decisions.
Testing: 2/3
The patient had just completed thorough testing in his previous ED visit earlier that day, so no further lab testing was completed. The physician is able to demonstrate that he reviewed this testing, by documenting that the INR was 1.5. One criticism is that the physician did not elaborate about his reasoning to not order a CT scan. Failing to describe your rationale for NOT ordering a relevant test is one of the most common documentation pitfalls.
There are some indirect clues about why he didn’t order a CT. “Without concussion” indicates that he may not think the fall was very serious or had caused any significant injury. “INR 1.5” shows that he does not think the patient is fully anticoagulated. These are helpful clues but only dropping mere hints about decisions of this magnitude will leave a physician wishing they had better documentation if the case ends up having a bad outcome.
Therapy: 3/3
The patient was given a tetanus booster. There is no specific documentation about this decision, which is reasonable, because it is an obvious and logical intervention. With hindsight, it is obvious the patient needed reversal of his anticoagulation, but this is outside the scope of the documentation review.
Differential: 2/8
There is no explicit differential documented, although it is possible to make some inferences about the possibilities that the physician considered. The only specific disease entity that the physician mentioned is a concussion, which he has ruled out. Ideally, the differential should consistent of other things that have been ruled out. This could have included causes of the fall (syncope, seizure, etc…) as well as effects of the fall that have been ruled out (basilar skull fracture, facial fractures, cervical spine fractures, etc…). The easiest way to address this is to document what relevant disease processes have been ruled out solely based on the history and physical.
Discrepancies: No deduction
Any discrepancies between the physician note and nursing or EMS notes will be closely scrutinized. No obvious or significant discrepancies are present in this case.
Aftercare: 3.5/4
The aftercare documented for this is case is very reasonable, when operating under the assumption that the patient does not have a head bleed. The plan of care is to observe the patient at home. This could be improved slightly with a brief description of what the patient was told to watch for, and to return to the ED if he noticed any worsening. The follow-up instructions are clearly shown with a specific time frame: “urgent care Aug 4”, which is only 2 days away. His scheduled appointments are also printed on the discharge instructions.