Home Page
Case 1: Shortness of Breath
Case 2: Fever
Case 3
Introduction
Outcome
Deposition
Legal
Documentation
Medical Review
This post will review the documentation of the doctor who treated this patient for a heroin overdose and discharged her several hours before her death. We’ll use the Documentation Rubric to grade the note. If you want an easy-to-use aid for writing good notes while you’re on your next shift, see the Documentation Template. The documentation in this case has several areas that are worth highlighting, some positive and some negative. The first issue here is the use of T-sheets. While T-sheets are a fabulous way to document quickly and efficiently, they often contain a paucity of information. T-sheets are notorious for creating documentation that is very difficult to defend.
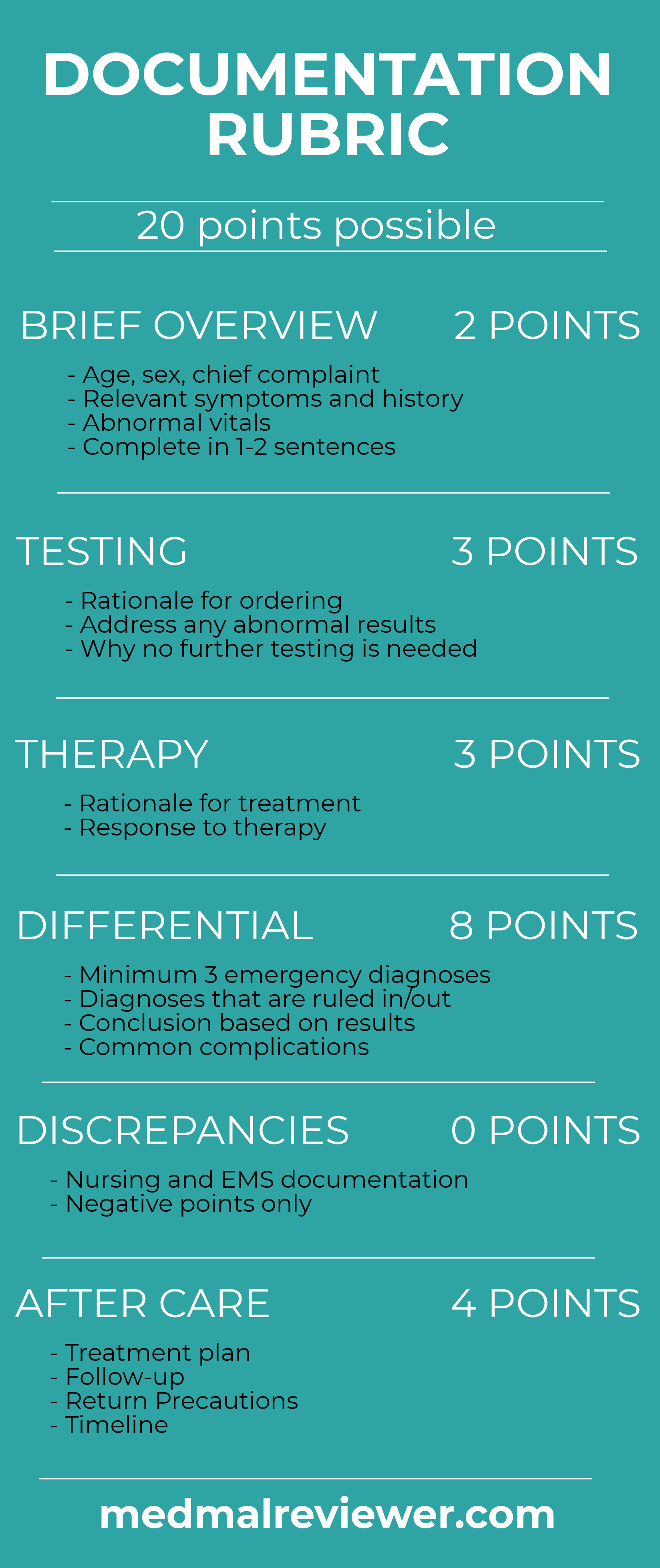
Remember that this is a purposefully difficult grading scale. Most notes do not meet all of the criteria, but they should strive for a full 20 points. This is difficult for many physicians to accept because they have spent their entire academic careers scoring top grades, and suddenly are faced with low scores created by this rubric.
This chart achieved a score of 9.5/20 on the Documentation Rubric.
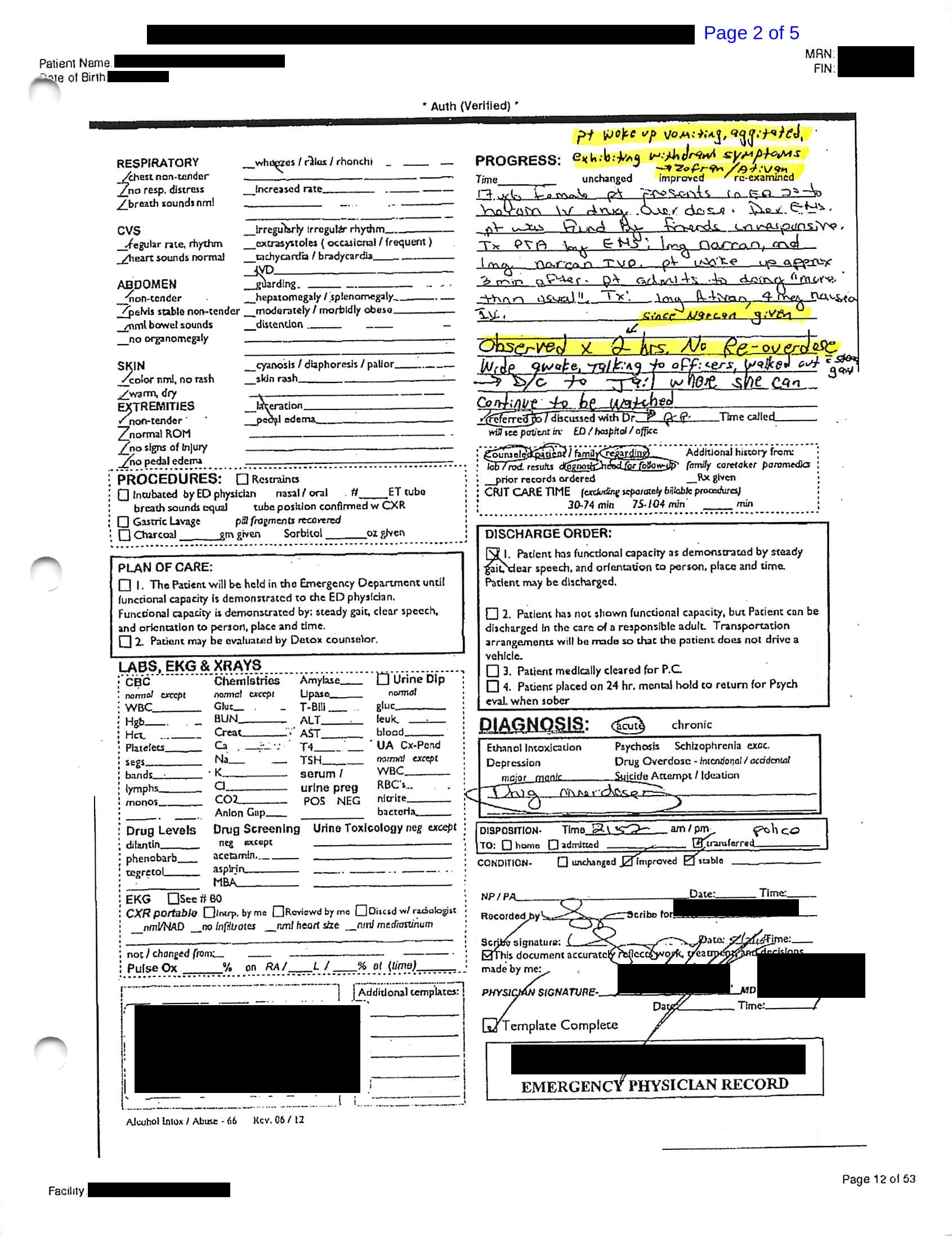
For easy reference, the physician’s chart is shown again here:
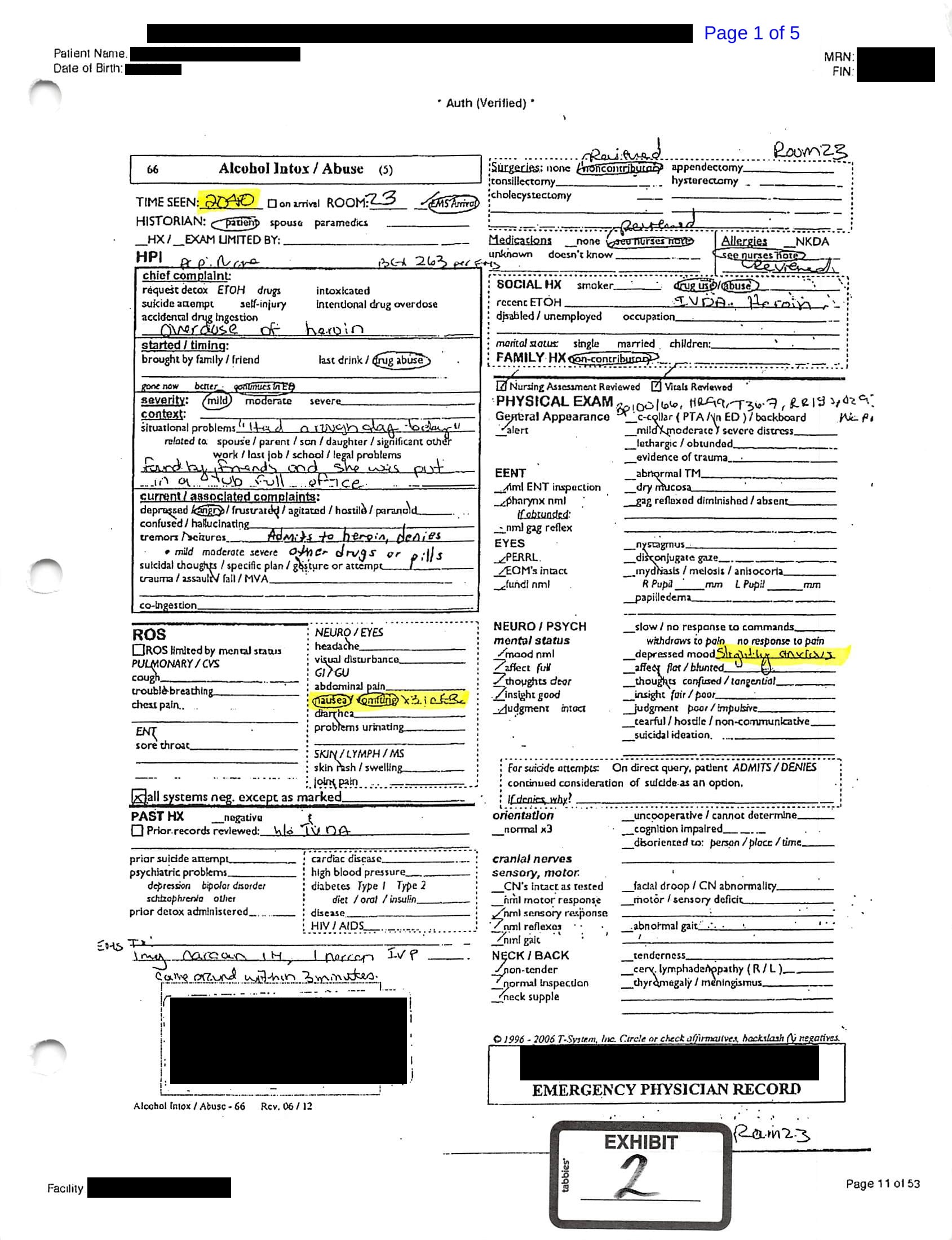
Brief overview: 1.5/2
A brief overview is present. The only things that could potentially be added would be the vital signs on arrival. This should not be a copy/paste approach, it should just be a short description to demonstrate that the physician has actually noted the vital signs, for example “17-year-old female patients presents to the ED conscious but tachycardic and hypoxic following heroin IV drug overdose treated by EMS with Narcan.”
Testing: 2/3
The physician needs to justify why particular testing is needed or not needed. One point was deducted here because the physician did not explain why no testing was needed. It’s completely fine to order no tests if none are needed, you just need to justify it. In this case, no lab or radiographic testing is needed because the most likely diagnosis is clear from history and physical. There are no further remaining diagnoses that are being considered that cannot be ruled out without lab testing. Furthermore, the patient already had a glucose showing she wasn’t hypoglycemic.

Therapy: 2/3
Any treatment that a patient receives should be noted. This is well done in the chart. We can clearly see that the patient was given Zofran because they were vomiting. The physician’s thought process is clearly explained (and even if not, obviously inferred by any reasonable medical provider). We can see that the patient was given lorazepam for withdrawal in the note at the very top of the progress section. The rationale behind why the physician ordered this therapy is clear, even if it is questionable (we will review why benzodiazepines are not a wise idea for this patient in the following post on the medical management). The therapy section of the Documentation Rubric also assesses any documentation about the patient’s response to the treatment they have received. At discharge the patient is described as feeling better, although a brief description of specifics would be helpful.
Differential: 2/8
Any EM doctor’s note needs to indicate that a differential was at least considered briefly, even if the diagnosis is obvious. This note has basically no evidence for consideration of other disease processes besides overdose. There is a brief mention of “withdrawal” but no elaboration. A differential diagnosis of one item is insufficient. Even when the diagnosis seems absolutely certain, physicians can build a differential based on diagnoses that they have already ruled out. Here are some mental approaches to building your differential and avoiding the trap of only documenting one thing:
- Consider the 1-2 sentence case summary listed at the very beginning of the MDM. Think about that sentence in isolation, not all the other details you have collected. Boil the situation down and oversimplify it, then build a differential from there. The differential is a rapidly changing/evolving list; it is not static. It is very broad at the beginning and gets rapidly narrowed subconsciously even if you only glance at the patient. Try to go back and remember what diseases you were considering at the very beginning, when the differential was very broad.
- Ask yourself: What would any board-certified EM doctor consider in that situation if they only heard the brief summary?
- Document similar things that the patient clearly does NOT have based on history/exam. In this case a physician could document why they do not think that various other drug overdoses caused the patient’s presentation: benzodiazepines, synthetic cannabinoids, methamphetamines, mixed overdoses, etc… A good differential includes diagnoses via positive (diagnosis that the evidence suggests) as well as diagnoses via negative (diagnosis that were considered but are now ruled out by the evidence).
- Another useful cognitive exercise is to comment on frequent complications of the obvious diagnosis. In this case the worrisome complications of IV drug abuse would include things like bacteremia, endocarditis, etc..
- Other medical diagnosis not related to overdose should be considered: hypoglycemia can cause nearly any symptom and it should be commented that this was likely not the case because EMS had an elevated blood sugar level. Pontine stroke can cause pinpoint pupils and unresponsiveness, but it should also be commented that this is very unlikely given the fact that an alternative diagnosis has been identified that is far more likely.
- Another consideration in this case would be a suicide attempt by the patient. If this patient was actually trying to commit suicide, it would drastically change their management.
When documenting a differential diagnosis, it’s a good exercise to make yourself come up with at least 3 items. Anyone can use the cognitive tricks above to build a long differential of items that have been considered and ruled out, and things that have been ruled in. Every thoughtful physician is already doing this process mentally, but recording it will make the documentation much more defensible.
In some cases, patients are harmed because a full differential was not considered. The above cognitive tricks may help physicians avoid missing a diagnosis. Not all bad outcomes or malpractice cases are due to short differentials leading to bad outcomes, but building a differential is a worthwhile practice that will improve your documentation and make you a better clinician.
Aftercare: 1/4
There are 3 pillars to aftercare: plan of care, follow-up, return precautions. They all need to have explicit time frames. For example, a child with otitis media who has been given antibiotics needs to have a time frame for the antibiotics (7 days), time frame for follow-up with pediatrician (3-5 days), and to immediately return to the ED if certain criteria are met. In this case, the physician clearly has indicated that follow-up with PCP is recommended. Unfortunately, there is no time frame indicated. The only plan of care listed at this point is follow-up with an unclear time frame. We will review other plan of care options in a coming post about addiction (addiction center referral, suboxone, naloxone prescription, etc…). Return precautions were not discussed. All discharged patients need to know what to watch out for and what to do about it. This is usually comprised of the emergencies that are unlikely but could occur, and they should immediately return to the ED for these findings. Furthermore, if the patient will not be taking care of themselves, this information needs to be given to the person taking care of them.
Discrepancies: No point deduction
Any discrepancies between your chart and the EMS or nursing chart should be addressed. It looks bad when a lawyer discovers completely different information between the documentation. If possible, confer with the author of the other notes so that they all reflect the true situation. If not possible, directly chart what part you disagree with. The T sheet indicates that “nursing assessment reviewed”, and no glaring discrepancies were found, therefore no points were deducted.
Overall, this chart scores 9.5/20. Based on reviewing many malpractice cases, I would say that this is an average note. It is well within the normal standard for what atypical ER doctor would document. There is certainly room for improvement but it is not atrocious. The bad outcome does not seem to be related to the quality of the documentation, and even perfect documentation would not have prevented the patient’s death. Nevertheless, better documentation is easier to defend and helps build a mental approach that is thoughtful and thorough. Using the Documentation Template while you work will help contribute to better notes and better care.