The documentation in this case played a critical role in the outcome of the lawsuit. The attending did not bother to leave a note in the chart, leaving the resident to suffer the legal consequences by herself. He signed the chart days later, but unfortunately a signature does not qualify as documentation.
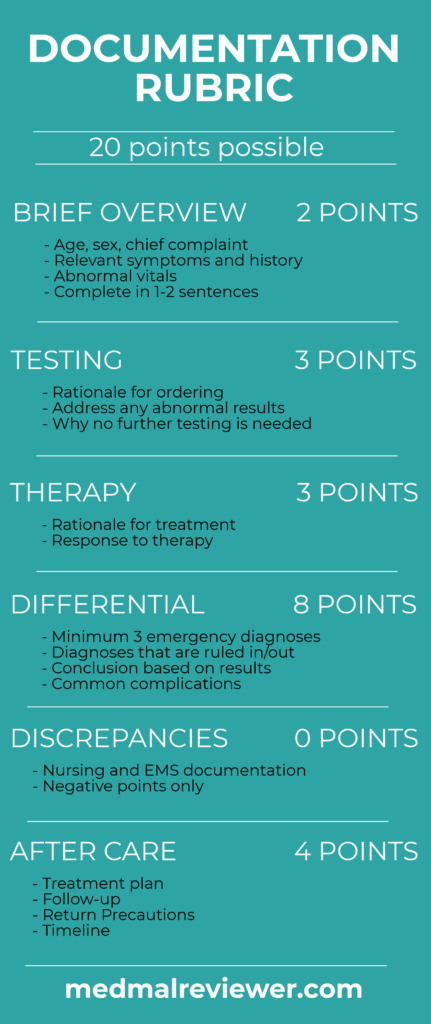
The attending’s note scored 0/20 points on the Documentation Rubric. This is the lowest score ever on a Med Mal Reviewer case.
In a twisted sense, the attending successfully dodged all responsibility for the bad outcome. However, avoiding culpability in this manner is unacceptable. Rewriting an entire note is not necessary for a supervising physician, but at the very least a sentence attesting to the documented history and exam is necessary.
The resident’s note was much better than the attending’s note, simply on the basis that she actually wrote one.
Her note scored 10.5/20 points.
The Documentation Rubric assesses only the part of the note that addresses the physician’s overall assessment and decision-making. It does not assess the history, review of systems or physical exam. In the resident’s note, the relevant section is titled “Assessment and Plan”.
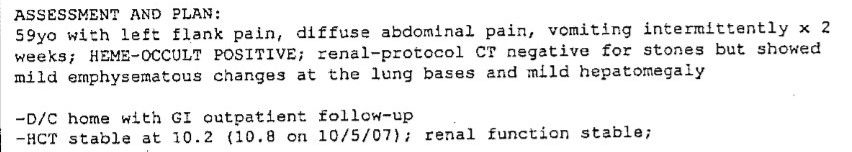
Brief Overview: 2/2 points
The age and chief complaint are all listed with a brief description of his symptoms. There are no abnormal vitals that need a comment. This information is described in one sentence.
Testing: 1.5/3 points
The tests that had abnormal results are listed. She briefly describes the positive hemoccult result and the CT scan result. This is a vastly preferable approach to the usual EM habit of copy/pasting hundreds of lines of labs and imaging results. Do not copy/paste lab and imaging results into your note. It creates unnecessary clutter with information that readers can look up elsewhere in the medical record.
Points were deducted here as she did not comment on the drop in hemoglobin compared to more distant test results. Additionally, the reasoning behind ordering a non-contrast study is not clearly addressed. Both of these issues were key factors in missing the aortoenteric fistula.
Therapy: 1/3 points
There is no mention of pain medication, fluids, antiemetics or any other treatment in the chart. If medications are given for logical reasons (analgesics for pain;, antiemetics for nausea, etc…) then no explanation is required. However, a brief note about how the patient responded to these medications is helpful. It shows that the physician reassessed the patient and will be viewed favorably by a jury.
Differential: 2/8 points
This note lacks a good differential. There was obviously concern for a kidney stone based on the CT scan that was ordered. There was a final diagnosis of gastritis noted. Screening was done for worsening anemia. There was a brief note made about upper or lower GI bleeding, although this essentially amounts to re-documenting the patient’s symptoms rather than a differential.
An EM differential should focus on the emergency diseases, and there should have been explicit documentation about the possibility of an aortoeneteric fistula. In a patient with vomiting, abdominal pain and history of a major vascular surgery, the physician should at least document that they thought about an AEF.
Remember that one of the most important parts of documenting an EM differential is making a note of the relevant emergencies you think the patient does NOT have. If the physician truly felt that this patient did not have an AEF, they should have stated it in their note.
Discrepancies: No points deducted
There were no major discrepancies between any nursing, EMS or physician notes.
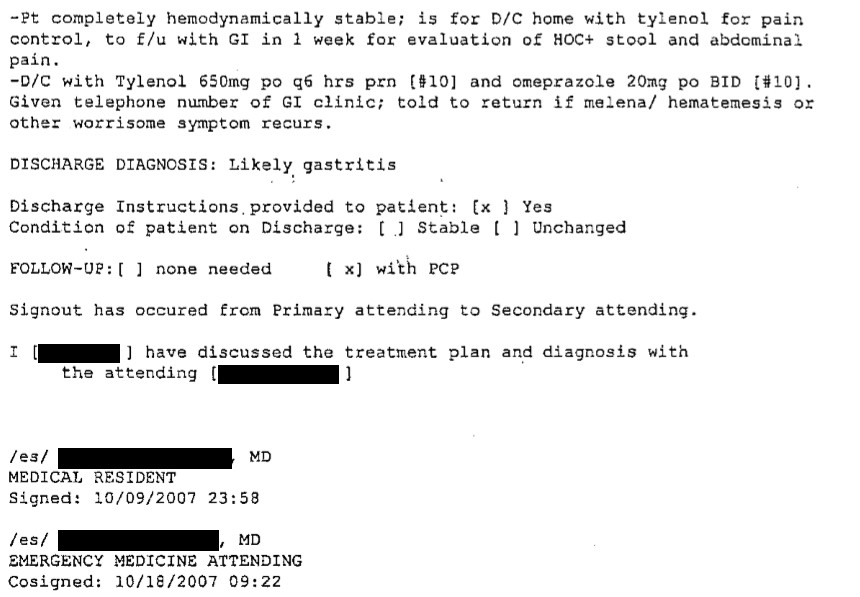
Aftercare: 4/4 points
The plan of care following the patient’s discharge is well documented. The patient is given instructions to take Tylenol and omeprazole for his symptoms with clear instructions on dosing and frequency. He was set up with a GI appointment within one week. He was given the phone number for the GI clinic. The patient was instructed on reasons he would need to return to the ED.
The resident hit all 3 points of a safe discharge planning: home treatment (medications included dosing and timing), follow-up instructions (including the phone number for the GI clinic) and return precautions.
A score of 10.5 may seem low, but it is quite impressive that this off-service resident was able to get this many points. The Documentation Rubric grades EM physicians to a perfect standard. Even in everyday practice, achieving a perfect score is not necessary. The Rubric is an aspirational target, not a benchmark that needs to be hit on every patient.
Case 14 Take Home Points
– consider aortoenteric fistula in patients with the appropriate surgical history
– order CT scans with contrast if concerned about AEF or other vascular pathology
– do not be falsely reassured by a stable hemoglobin in diseases that can have a herald bleed
– attending physicians must provide brief documentation even when a resident writes the note, simply signing a note is insufficient