The purpose of this website is to improve doctor’s medical knowledge and documentation by reviewing real-life malpractice cases. This article will review the documentation of the physician who was sued. There are three goals of documentation: defensibility, continuity of care, and billing. This post will focus primarily on the defensibility aspect of documentation. I have created a Documentation Rubric that will help guide the grading of this note. I have also created a Documentation Template to help physicians write defensible notes.
Home Page
Case 1: Shortness of Breath
Case 2
Post 1: Introduction Pt 1
Post 2: Introduction Pt 2
Post 3: Introduction Pt 3
Post 4: Bad Outcome Pt 1
Post 5: Bad Outcome Pt 2
Post 6: Legal Outcome
Post 7: Documentation Review
Post 8: Medical Review
This case had several bounceback visits across multiple different facilities, producing multiple notes. Given that this blog primarily focuses on ED documentation, the focus will be on the ED notes, specifically, the note from the first visit. The urgent care has such limited information that it is hardly even worth taking it through an evaluation with the documentation rubric.
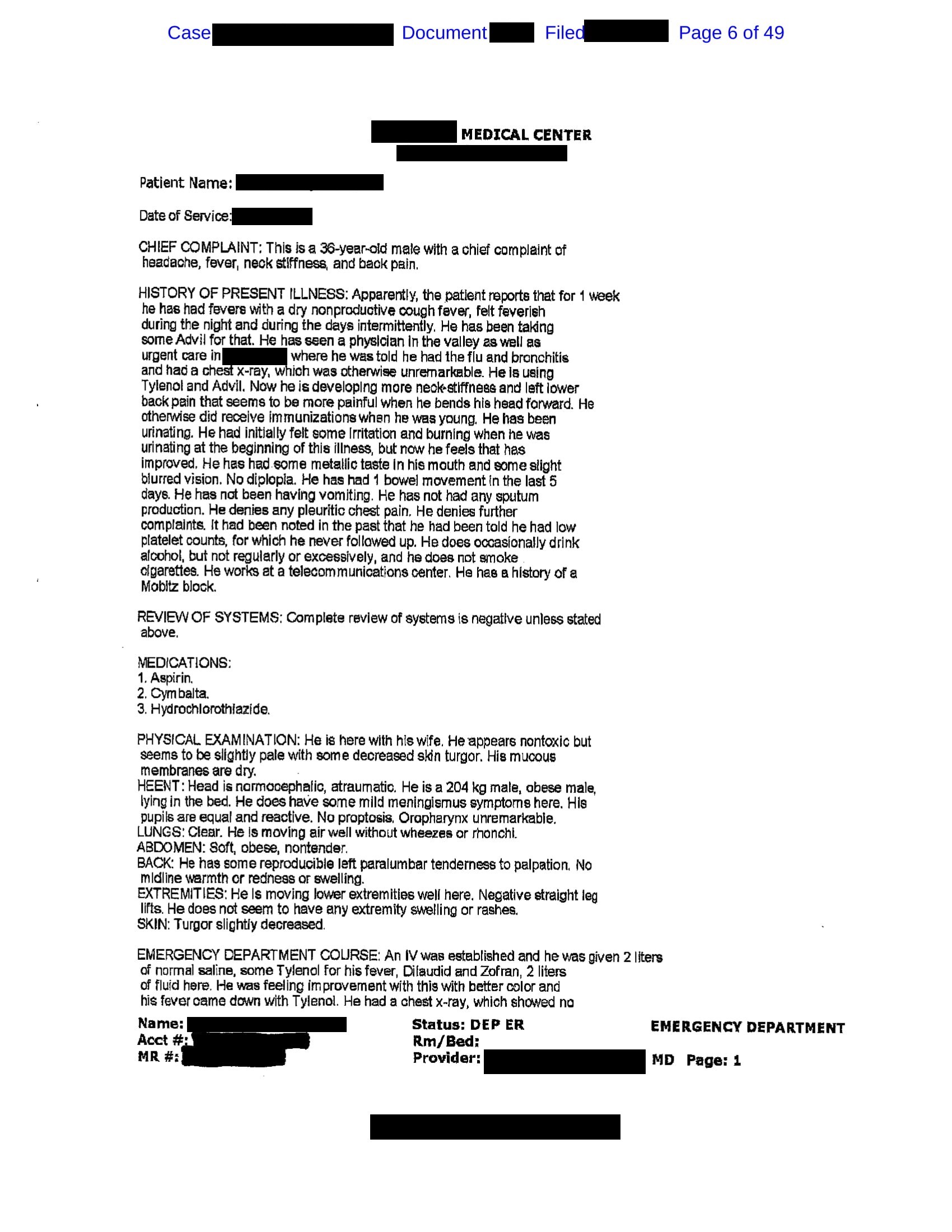
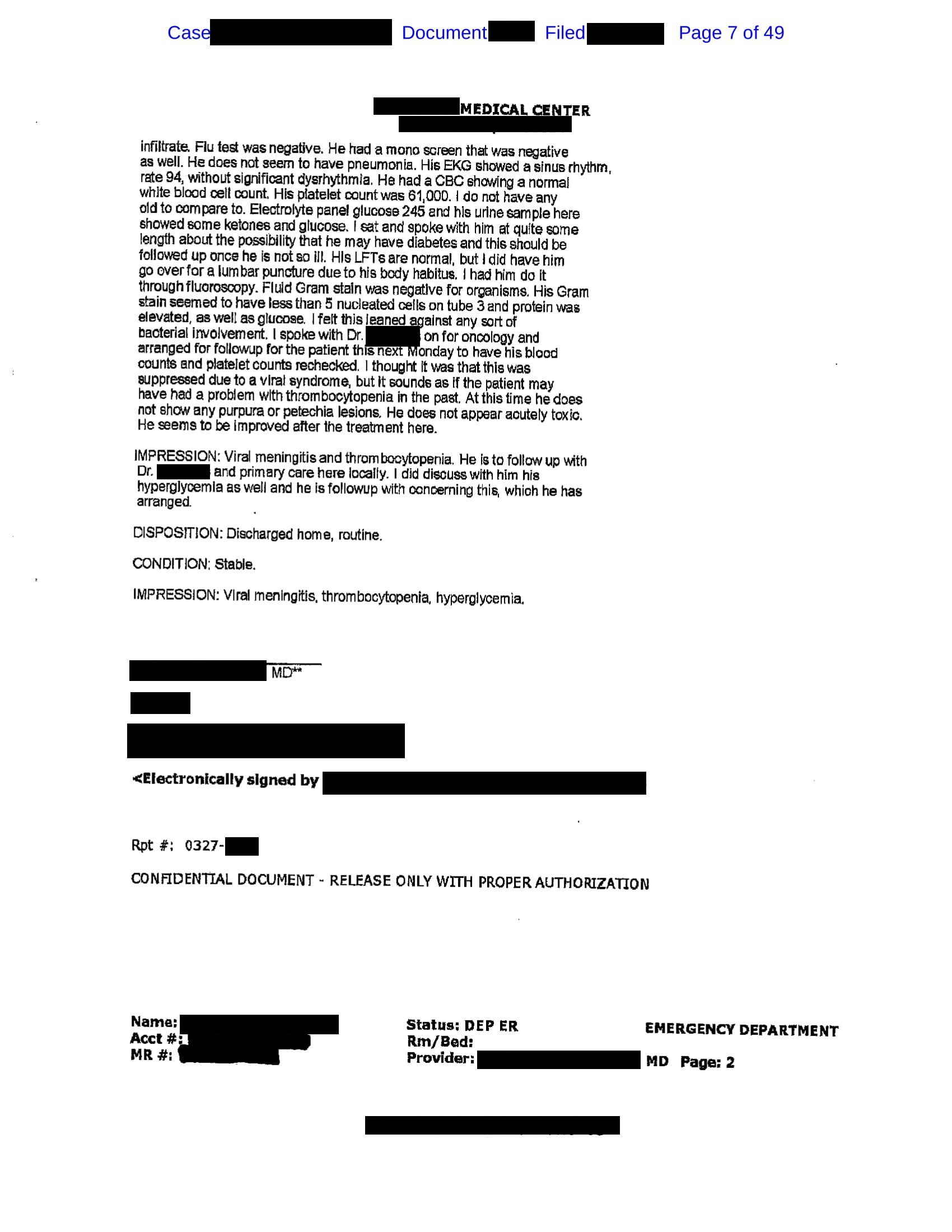
The note documented at the first ED visit is shown again here:
The review of the documentation will focus just on the documentation. The medical issues will be addressed in a subsequent post. Just like a math professor may give credit for showing work that still ends up at the wrong answer, we will give documentation credit even if the final diagnosis is incorrect.
This note contains an ED course and an impression, although not a clearly-labeled medical decision-making section (MDM). When I say “MDM”, I mean the part of the note where the doctor describes their thought process about the patient. The name is less important than the simple fact that your thought process is described somewhere in the note. Different doctors and different EMRs put information in various places and give it various names. In my opinion its best labeled “medical decision-making” and located at the end of your note, but I understand that there are many approaches to how notes are structured. The Documentation Rubric doesn’t punish anyone just because your notes are organized in a different manner. Try out the Documentation Template to see one method to organize your notes in a way that will help you document well.
This note achieved a score of 14/20 on the Documentation Rubric.
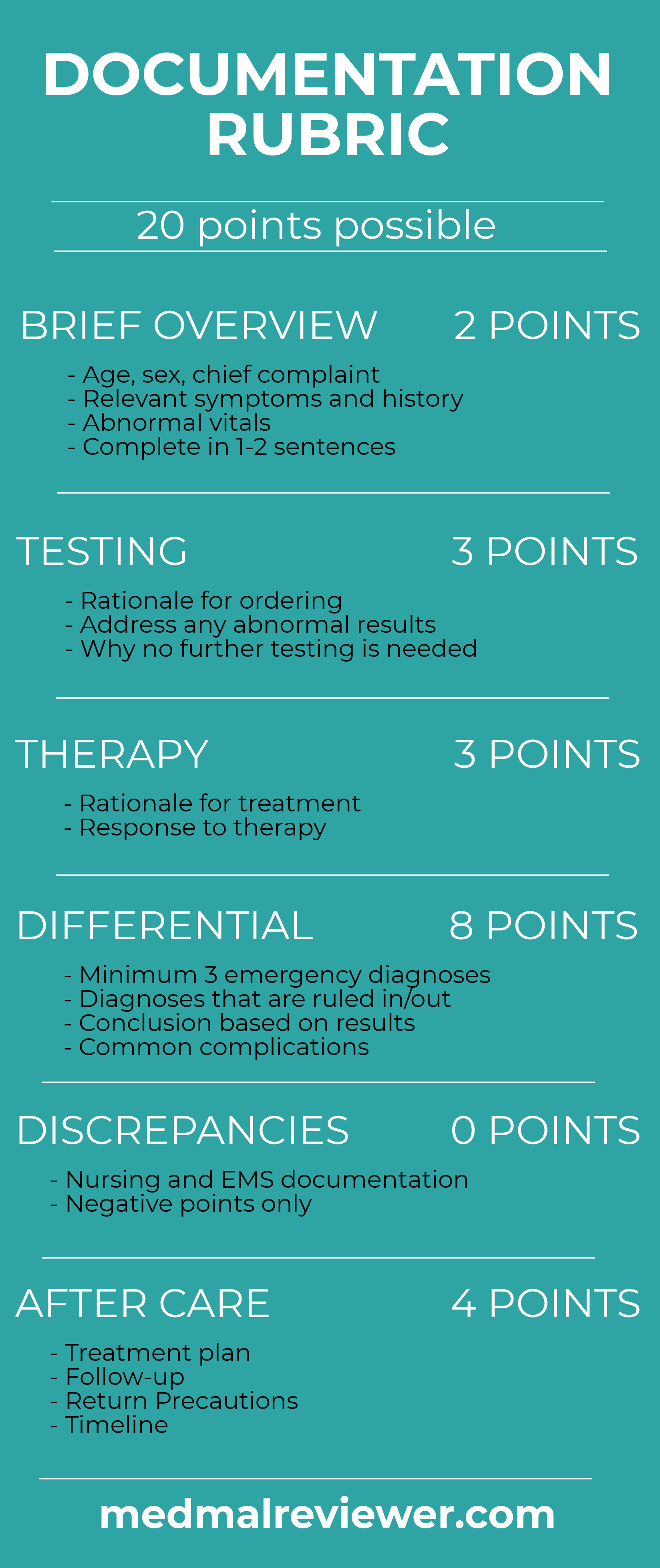
Brief Overview: 2/2
The note does in fact contain a very effective brief overview sentence. While it is not found in the ED course or impression, it is clearly listed in the chief complaint and deduced from other parts of the note. Recall from the documentation rubric that the brief overview should communicate the patient’s presentation in 1-2 sentences. This is something that ED physicians should excel at: condensing very complicated patient presentations down to a very brief summary. The emphasis here is the big picture while accepting the sacrifice of smaller details that can be included elsewhere.
In this note, this information is present but found under the chief complaint. Generally, the chief complaint should be the single symptom that the patient is most worried about, but my consist of a constellation of symptoms. Sometimes this is fairly obvious, as commonly happens with chest pain. Other times, as in this case, the patient has various complaints and has difficulty choosing just one. If the patient is having problems boiling it down to a single issue, an effective technique is to ask the patient, “If I could fix only one symptom for you, which one would it be?”. The answer is the chief complaint. There is an art to this, it is not an exact science. It is not the patient’s fault if they have difficulty choosing one chief complaint, you are the physician and must assist them.
Another important part of the brief overview is an extremely brief description of the vitals (if significantly abnormal) or other noteworthy physical exam. The note does contain a brief mention of fever that has resolved, found in the ED course. Unfortunately, there are no documented vital signs in the note or description of other vitals. I have no doubt that the rest of the vitals are included somewhere else in the care, but in my opinion they should be included in the physician’s note if significantly abnormal. The vitals signs are, after all, VITAL.
All this information should be included at the start of the decision-making section. It’s a little fragmented here but I try not to deduct points just because things are organized in a way that I don’t personally like.
Testing: 3/3
The testing that is ordered follows very naturally from the differential (which we will review further down). The results are clearly described. Abnormalities are addressed. The rationale for what is ordered and how it is interpreted is overall quite good.
The main issue in the interpretation of testing is the interpretation of results that leads to a diagnosis of viral meningitis. This is where the line blurs from the testing section to the differential section. The diagnosis of viral meningitis is somewhat of a soft call, with CSF showing negative gram stain, normal WBC count, elevated protein, elevated glucose. At this point, it is not impossible for the patient to have a diagnosis of viral meningitis, but it is a stretch. In Emergency Medicine, we are allowed to discharge patients without a final cohesive diagnosis. Instead of discharging with a diagnosis, consider discharging with a symptom. Giving the patient a final diagnosis when it is somewhat uncertain is not necessary. Furthermore, it plants an idea in the head of the next doctor that can be difficult to ignore. You can help your colleagues avoid anchoring, set them up for success, and make it more likely that they will catch your mistake before it causes serious damage by using symptom-based discharge impressions.
Therapy: 2/3
The rationale for the therapy given is logical. It is clearly listed at the beginning of the ED course (although the 2 liters of fluid are listed twice). The reason for giving all of these medications is obvious. One very slight oddity is the fact that nowhere is the patient listed as being nauseated, but he is given Zofran. Dilaudid seems somewhat aggressive for a patient with multiple nonspecific symptoms including headache (opioids being a poor choice for headache), but unfortunately is still consistent with what many ED physicians would do.
Especially good is the fact that the response to this therapy is documented. Often times, physicians working in a busy environment overlook documenting a re-evaluation. This physician is able to describe an improvement in his condition after this therapy, which is reassuring. Documenting a second assessment and response to treatment is a critical part of defending your care.
Differential: 6/8
As a general exercise, it is smart to include at least 3 diagnoses in the differential. As an ER physician, you should make an effort to include at least 3 EMERGENCY diagnoses in your differential. Granted, there are some patients in which the differential is less relevant. For example, a patient who comes in mid-delivery with a crowning baby. The diagnosis is obvious. However, these cases are few and far between. A common reason for missing a diagnosis is “I never considered it”. When you say to yourself “there is literally nothing else this could be”, you are setting yourself up for failure. Document a one-item differential at your own risk. Here are some cognitive tricks to improve your differential:
- Consider other organ systems. Often times people get mentally trapped into only thinking about the diseases within one organ system. Entertain if this could be musculoskeletal, cardiovascular, infectious, autoimmune, neoplastic, etc…
- Consider other anatomical compartments
- Find any abnormal result (labs, imaging, EKG, etc…) and consider a differential for that abnormality in isolation.
- Consider parts of the presentation removed from the context of the rest of the patient. What is the differential for a 36-year-old man with back pain? Any EM resident could build a long differential of emergency diseases for 36-year-olds with back pain.
- If you can only think of one item in the differential, consider the common complications of the one diagnosis. If the patient has an obvious fracture, consider neurovascular compromise, compartment syndrome, open fracture.
- Document diseases that the patient obviously does not have, and why its obvious that they don’t have them.
- Be explicit. Don’t document “there’s no infiltrate”. Document that there is no infiltrate and therefore this does not seem like a pneumonia. Most people reading your chart will know what you were thinking, but it is better to clearly describe it.
- Consider the aorta.
Another tip: I try not to document that a disease is impossible. I only speak in terms of likelihood. I might say something is extremely unlikely, but I try not say that they absolutely do not have it, or that it is impossible to have a particular diagnosis. Anything is possible.
This patient has a robust differential documented. There is explicit mention of influenza, mononucleosis, pneumonia, dysrhythmia, diabetes, bacterial meningitis, viral meningitis, viral syndrome. There is also thoughtful review of his abnormal lab tests including hyperglycemia and thrombocytopenia.
Overall, this is a very good differential. There are multiple emergency diseases considered. One area for improvement would be consideration of other organ systems, particularly musculoskeletal. An ED doctor considering a patient with back pain and fever should be considering spinal cord pathology, and there is no mention of this aside from meningitis. The physician did indeed include a consideration of a diseases process that was both neurologic, affecting the spinal cord, and infectious in nature (meningitis) but did not consider another diagnosis in this category that turned out to be the true diagnosis. Points are deducted because the differential could have been broadened even further, and for somewhat suspect interpretation of the CSF results.
Discrepancies: No point deduction
Unfortunately, this case does not include nursing documentation as part of the legal exhibits. Therefore, there is no way to tell if any discrepancies were present. EMS was not involved.
Aftercare: 1/4
The 3 main areas of aftercare are the plan of care, follow-up, return precautions. They all need well-described time frames. The physician has documented that he “sat and spoke with him at quite some length about the possibility that he may have diabetes and this should be followed up once he is not so ill”. The fact that there is documentation of a long discussion with the patient shows that the physician is thoughtful and kind, which will be looked favorably upon by a jury. Unfortunately, the focus of this discussion is inappropriate for the ED. Diagnosing type II diabetes is concerning but is very unlikely to be a primary emergency if there are no associated complications. This is a diagnosis for his primary care doctor, not the ED physician. Furthermore, the follow-up timeline for this is “once he is not ill”. This is not an inappropriate timeline from the ED. We want patients to come back to the ED or go to their primary doctor if they are still not improving. The primary care follow-up or ED return precautions should be focused on what to do if still not getting better or getting worse. What the patient needs to do once they’re better is far less important. The instructions to follow-up with their primary care doctor “once he is not ill” are probably given from the mental framework of diabetes testing, which is misguided in this case.
One positive note is that the physician set up follow-up with a specialist. It is somewhat odd that a heme/onc doctor was selected as the appropriate follow-up, given that the thrombocytopenia seems to be a minor abnormality. However, it does show that the physician was not flippant or cavalier, and did actively consider the follow-up plan.
There is no plan of care in regards to medication or behavioral regimen to help manage the symptoms. There are no instructions documented in regards to what would need return to the ED. The follow-up with oncology has a time frame listed (“next Monday”), but nothing else has a time frame.
Overall the documentation was quite good in this case as compared to many malpractice cases I have reviewed. The physician was thoughtful and thorough in their care and it was well-documented. Area of improvement include a slightly more robust differential, using symptom-based discharge plan as opposed to definitive diagnosis, and improving the aftercare instructions.