Index Case 7
Ankle Injury
Testing and Treatment
Disposition
Billing
Return ED Visit
Outcome
Plaintiff Claims
Defense Response
Legal Outcome
Case Review
Documentation Review
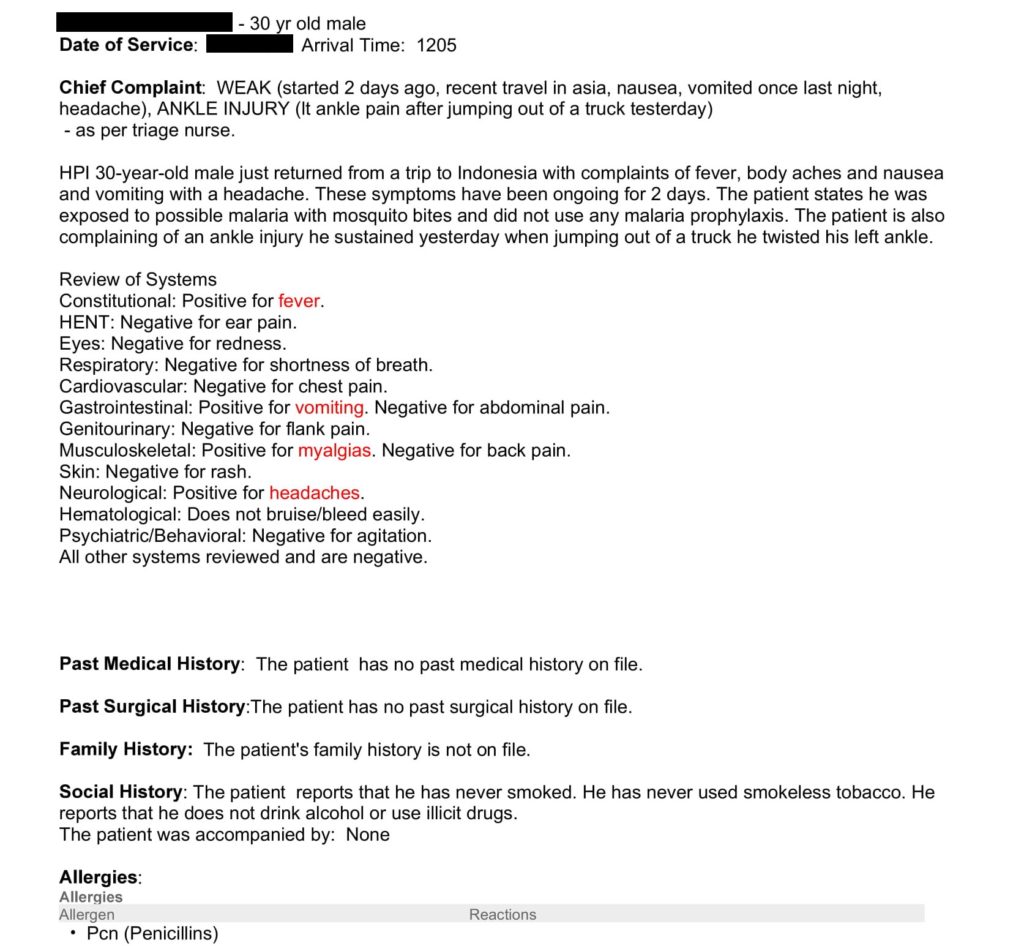
This month we will be reviewing the documentation from the initial ED visit. It is shown below for reference.

In order to assess the note, we will be using the Documentation Rubric. If you are looking for a structured way to write fast, defensible notes on your next shift, use the Documentation Template. The Rubric is for grading notes, the Template is for writing notes.
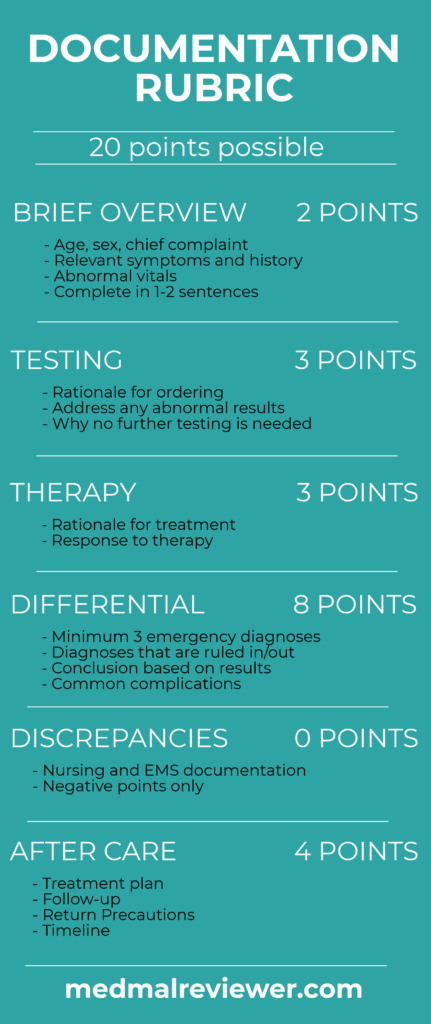
The physician’s note earned a score of 18.5/20.
This note was one of the best reviewed on this site to this point. It contained complete information and had a thorough explanation of the physician’s thought process. In fact, it was good enough that the hospital’s attorney was able to effectively use it to get the federal civil case dismissed. No doctor is able to predict when they are going to be sued. Writing good notes on every patient is important to enable your defense when faced with a lawsuit or adversarial chart review.
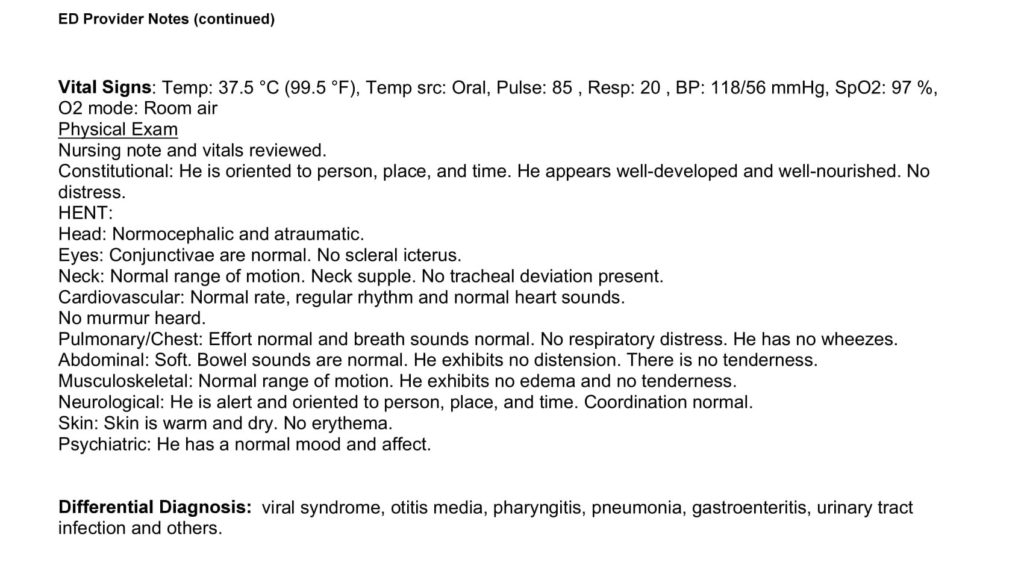
Brief Overview: 2/2
The note contains an effective brief overview, although it is listed as the first sentence of the HPI. The brief overview should be the 1-2 sentence explanation of the relevant facts related to the patient’s presentation. Basic explanation of their symptoms, any relevant PMH, and any markedly abnormal vitals should be mentioned. This is an excellent way to distill a patient’s complicated presentation into a brief summary.
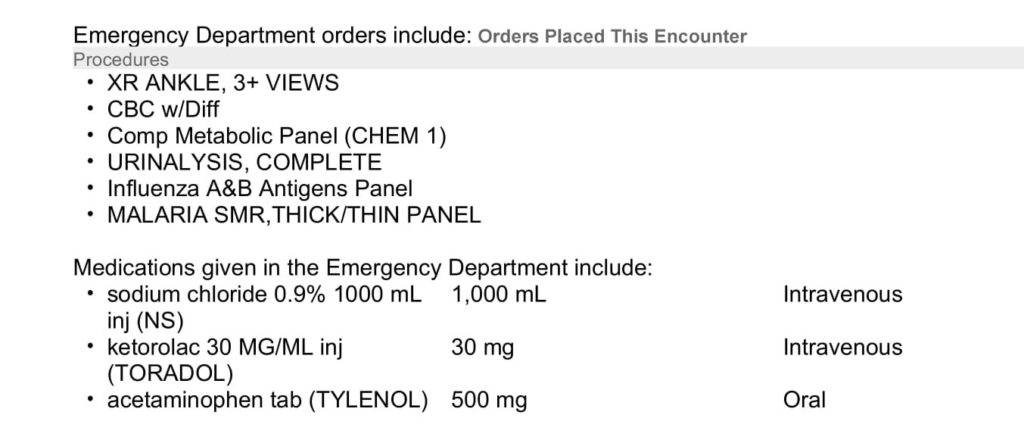
Testing: 2/3
The testing the doctor ordered is listed in their note. It does not need to be copy/pasted into the MDM or ED course, but relevant parts deserve a comment in the MDM. The note mentions malaria and influenza tests specifically, as well as the “significant” testing, and interpretation of lab and imaging tests. The bulk of these sentences are likely templated. These pre-written, templated sentences are better than nothing, but writing that describes this patient in particular is always more useful.
Therapy: 2.5/3
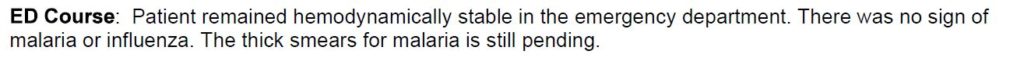
The therapy given (normal saline, ketorolac, and acetaminophen) is logical when considering the patient’s history and exam. The MedMalReviewer template does not require explanation when the medications ordered are easily understood. The response to the medication is described in the ED course, in that the patient remained hemodynamically stable. This demonstrates that the physician reviewed the repeat vital signs, which is a critical action when discharging a patient. Mention of change in the patient’s subjective symptoms could be made to improve this.
Differential: 8/8
This is one of the first notes that I have reviewed to actually include an effective differential. 6 separate disease processes are mentioned. In fact, the physician had a wider differential that he did not even mention, as he also tested for influenza and malaria (not included in the differential). Focusing on the emergency differential is preferable, but we all know that not all ED patients have an emergency condition. Therefore, including both emergency and non-emergency disease processes is wise.
Discrepancies: No deduction
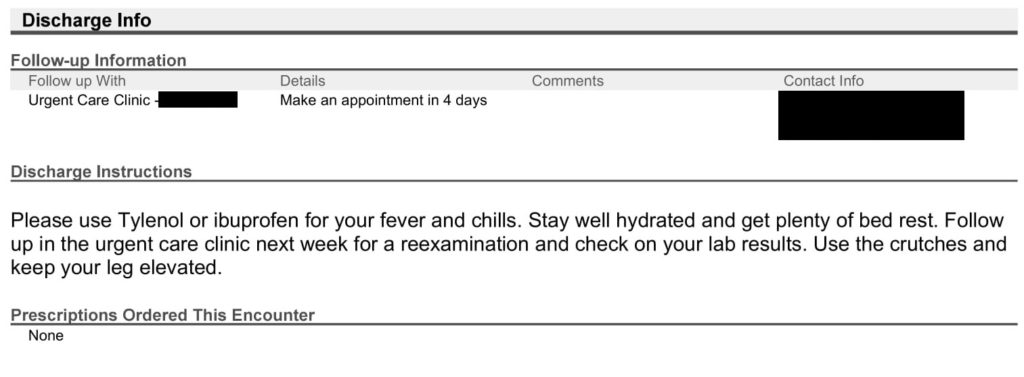
Aftercare: 4/4
This is an excellent set of discharge instructions. There were no specific time frames or doses of medications discussed, but this very well may have been included in discharge papers that the patient was given but not included in the lawsuit.
Return precautions are a protective mechanism for both the doctor and patient. They are the most critical part of the discharge process. They enable the patient by giving them information (ideally, both specific things to watch for and general instructions to return if anything changes), as well as protective for the physician. These instructions are ideally delivered twice: both in writing (so a patient can remember them and so they are documented) and in person (a verbal discussion between physician and patient augments printed discharge papers).
Fortunately for this physician, the patient did follow instructions and returned. The return precautions may have been the critical piece that saved the patient’s life. It is impossible to know what would have happened otherwise, but this lawsuit may have gone very differently for the physicians involved if the patient had not been given return precautions and had died at home.
Return ED Visit
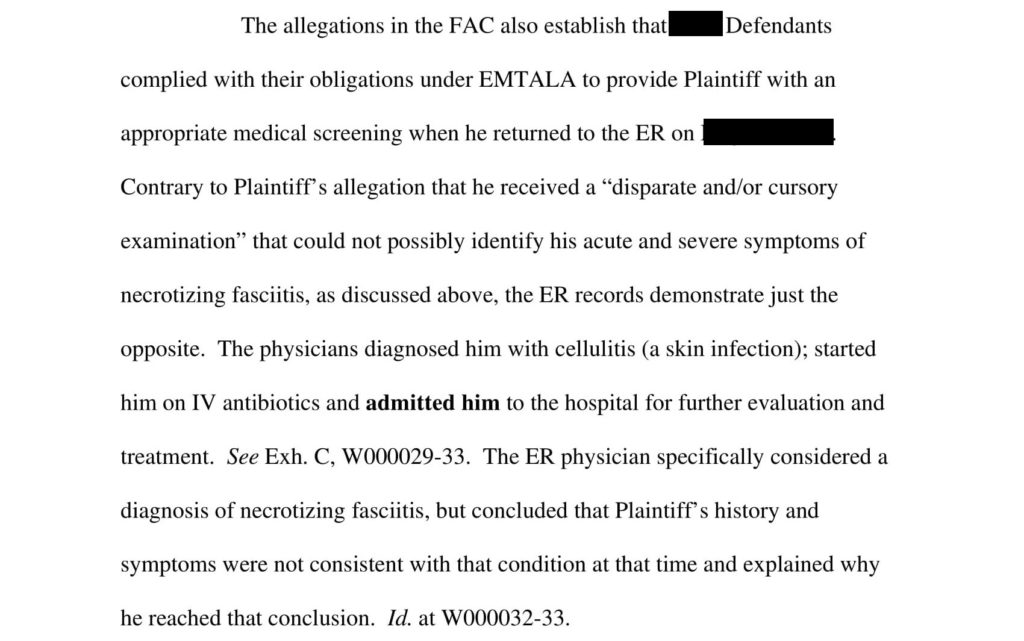
One surprising thing about this case was that the quality of both EM physician notes was very high. The second physician’s note specifically discussed their consideration of necrotizing fasciitis. This is excellent proof of the overarching goal of your note: describe your thinking. The physician thoroughly described his thought process, which helped establish a successful defense, even though he was wrong. For reference, his medical documentation about NF and the attorney’s opinion are shown below.
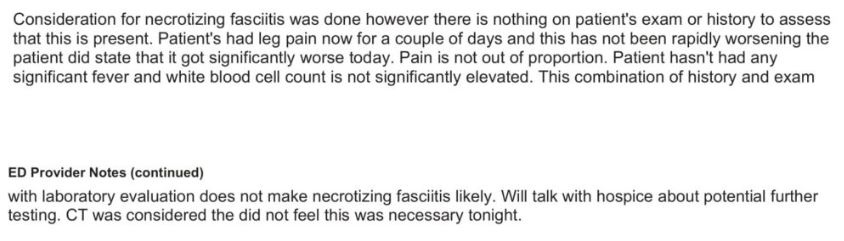
Attorney’s opinion:
Following the Documentation Template will result in high quality notes (just as those in this case), result in a very high Documentation Rubric score, and help your attorney achieve a successful defense.