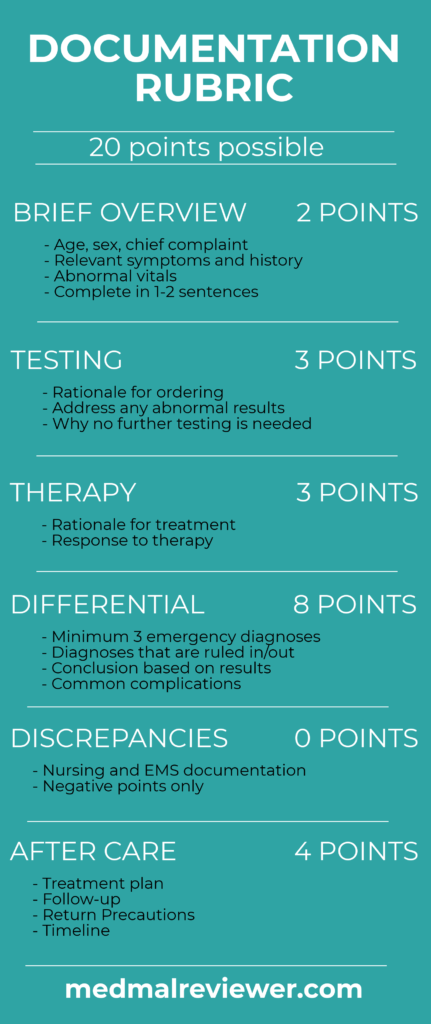
This case is unique in that the doctor was a general surgeon covering the ED. While he did not complete a residency in Emergency Medicine, the Documentation Rubric applies to any undifferentiated patient in the acute care setting.
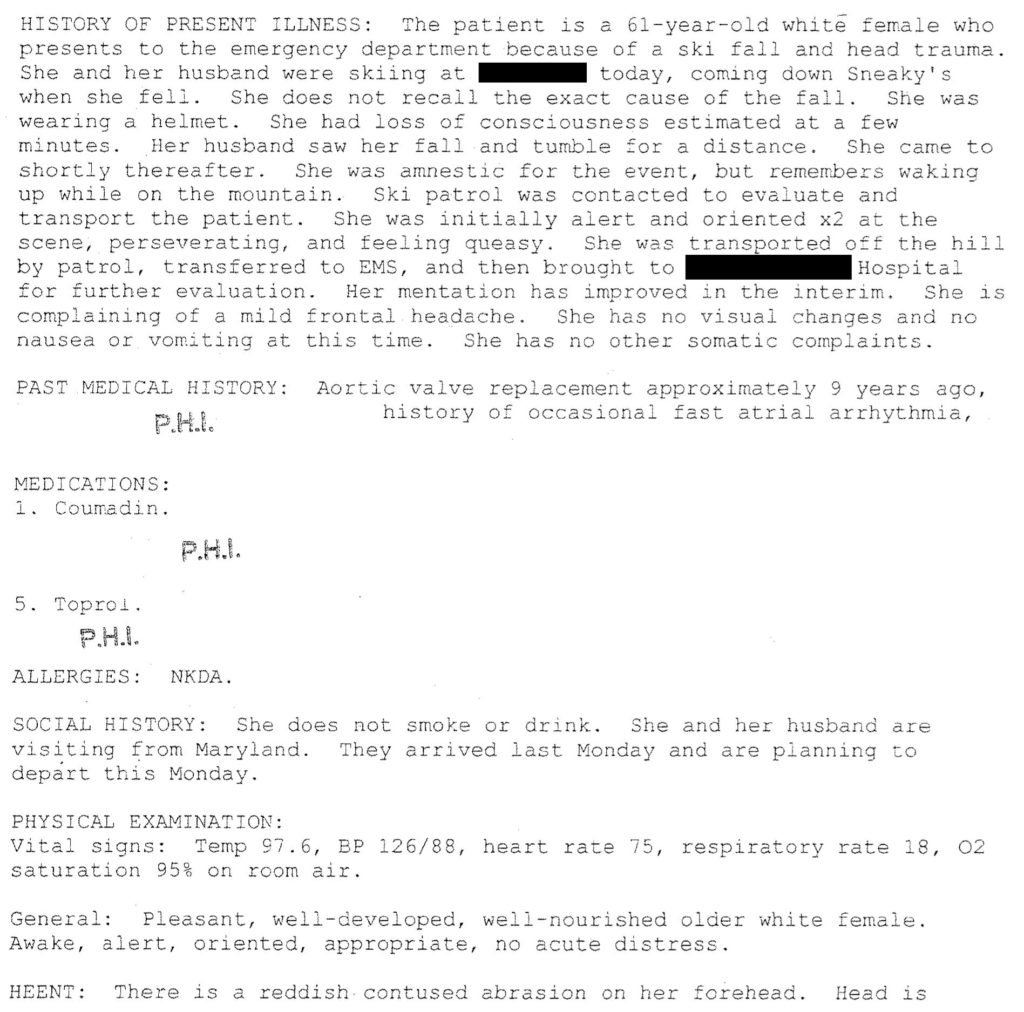
The note is very thorough and free of cookie-cutter text, which shows the physician to be thoughtful. His physical exam shows numerous findings that are specific to the patient.
The Documentation Rubric is used to assess the physician’s rationale and plan. This section of the note can have many different names (medical decision-making, impression, plan, ED course etc…). The rest of the note (HPI, ROS, exam) is for billing purposes and communication with other healthcare workers, and is not addressed by the Rubric.
This note scored 14/20 points.
Brief Overview: 1/2 points
All of the essential information is included in his chart. It is useful to give a 1-2 sentence summary at the beginning of the doctor’s rationale to show appropriate synthesis of the salient points. This is a MedMalReviewer style preference, but perfectly acceptable notes can be written without it.
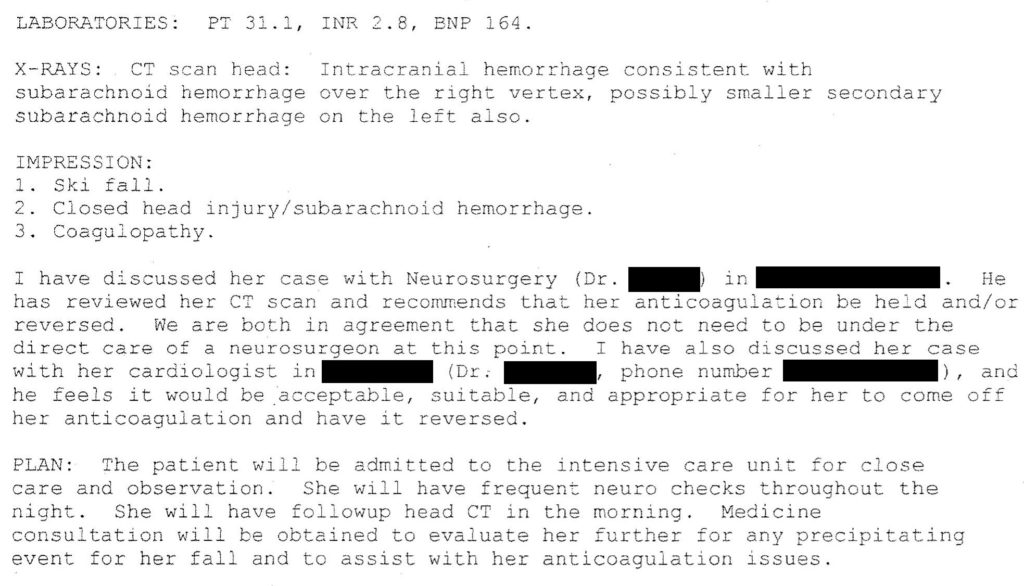
Testing: 3/4 points
This case does not hinge on whether or not the appropriate tests were ordered during her initial evaluation. The testing was appropriate and logical.
However, in order to write the highest caliber notes it is preferable to explain why you ordered the testing. In this case, she meets every clinical decision-rule criteria for a non-contrast head CT. This fact could have been briefly mentioned.
Another opportunity is to explain why no further testing was ordered. If the patient later is found to have other injuries, it will be useful to explain why other related tests were not ordered.
Examples could include reasons for not ordering a CT cervical spine, x-rays of chest or pelvis, extremities, etc…
It’s fine to not order more tests, just explain why.
Therapy: 2/3 points
The note mentioned reversal of anticoagulation but not further details. A brief note on which reversal agents he chose would be wise.
This case occurred in 2009, at which time fewer reversal agents were available.
Nonetheless, having to explain in his note why he gave 5mg of Vitamin K and did not give FFP initially may have triggered him to re-think he decisions before she deteriorated.
Differential: 4/8 points
The physician considered the obvious traumatic issues: head injury and the coagulopathy that made it more complicated. However, there is no indication that he considered other traumatic injuries or complications.
Many physicians would consider a head injury from a ski accident to be a severe mechanism, possibly consistent with a cervical spine fracture. The same could be said for intrathoracic or intrabdominal injuries, fractures, dislocations, etc…
I have no doubt that the physician thought about these issues and felt that they were unlikely. Why get imaging of any other area if there is no pain? It is a completely logical decision.
The problem is that lawyers (or your hospital peer review committee) reviewing the case later do not know what you were thinking. They can’t read your mind. Decisions that seem completely logical at the time are often called into question.
Make it easy to defend yourself by writing down a differential that includes injuries you think the patient might have, as well as related injuries you know they obviously don’t have.
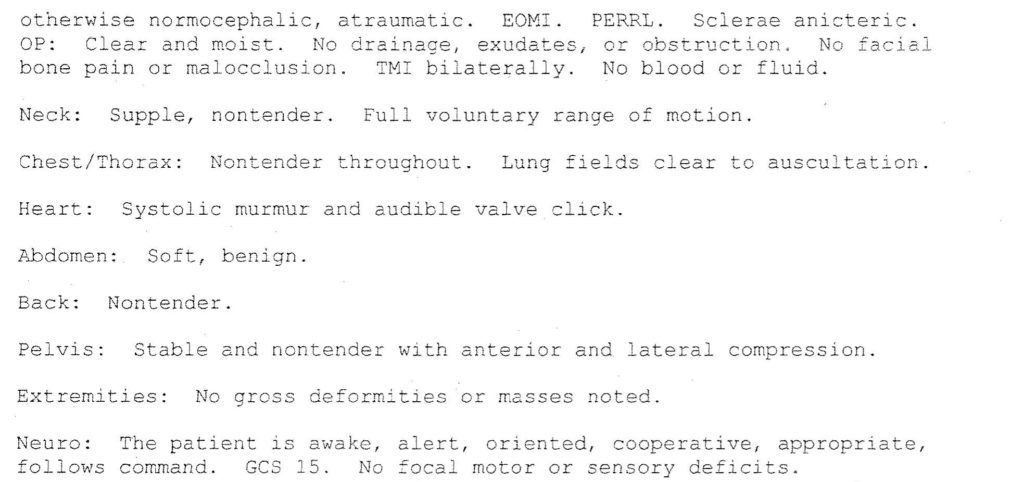
Discrepancies: None
There were no direct discrepancies during the initial evaluation between the ER nurses and the physician. Later issues would arise out of the allegedly delayed transfer from the ICU.
Aftercare: 4/4
The plan of care is clearly explained in his note. It is obvious to the reader that she will be admitted to the ICU. The doctor spoke with the neurosurgeon and they agreed that she could stay at the original hospital.
While the decision-making itself may have valid criticisms, his documentation of the consult and thought-process is appropriate.
Continue to the next page to see the final MedMalReviewer analysis.